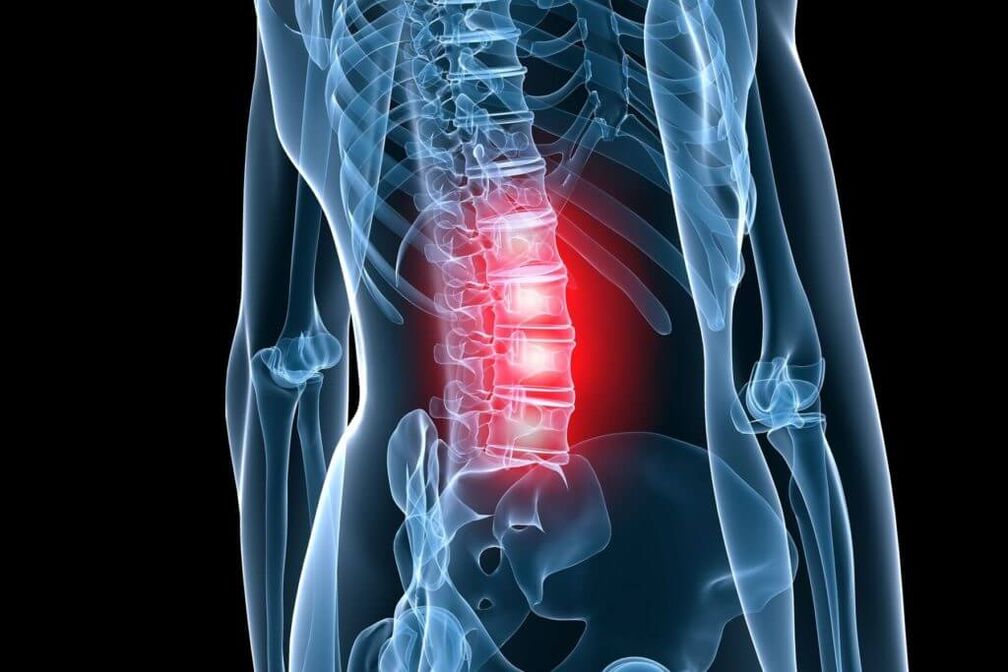
painFour out of five people experience a back at least once in their lifetime. For the working population, they areMost common cause of disabilityThis determines their social and economic importance in all countries of the world. Among the diseases that accompany pain in the lumbar spine and extremities, osteochondrosis occupies one of the main positions.
Osteochondrosis of the spine (OP) is a degenerative dystrophic disorder that begins in the nucleus pulposus of the intervertebral disc and extends to the annulus fibrosus and other elements of the spinal segment, with frequent secondary effects on adjacent neurovascularization. Under the influence of unfavorable static-dynamic loading, the elastic medulla (gel-like) nucleus loses its physiological properties - it dries up and becomes sequestered over time. Under the influence of mechanical load, the annulus fibrosus, which has lost its elasticity, herniated, and subsequently, fragments of the nucleus pulposus are dislodged from the fissure. This leads to acute pain (low back pain) because. The peripheral portion of the annulus fibrosus contains receptors for Luschka's nerve.
Stages of Osteochondrosis
According to the classification proposed by Ya. Yu, the intradiscal pathological process corresponds to stage 1 (stage) (OP). Popelyansky and A. I. Osner. In the second stage, not only is depreciation capacity lost, but fixed function is also lost as overactivity (or instability) develops. In the third stage, the formation of a herniated disc (herniation) is observed. According to the degree of herniation, disc herniation is divided intoelastic protrusionWhen the disc herniates uniformly, andisolated protrusion, characterized by uneven and incomplete rupture of the annulus fibrosus. The nucleus pulposus moves to these ruptures, forming local protrusions. In a partially prolapsed herniated disc, all layers of the annulus fibrosus are ruptured, and possibly the posterior longitudinal ligament, but the protrusion itself has not yet lost contact with the central portion of the nucleus. Completely prolapsed disc herniation means that not its individual fragments but the entire nucleus has prolapsed into the spinal canal. According to the diameter of intervertebral disc herniation, it is divided into intervertebral foramen, posterolateral, paramedian and median. The clinical manifestations of disc herniation are varied, but it is at this stage that various compression syndromes frequently occur.
Over time, the pathological process can move to other parts of the spinal motion segment. The increased load on the vertebral body leads to the development of subchondral sclerosis (sclerosis) and then the body increases the area of support due to marginal bone growth throughout the perimeter. Joint overload can lead to spondyloarthropathies, which cause compression of the formation of nerve blood vessels in the intervertebral foramen. It is these changes that are noticed in the fourth stage (stage) (OP), when there is complete damage to the spinal motion segments.
Of course, any patterning of a disease as complex and clinically diverse as OP is rather arbitrary. However, it is possible to analyze the dependence of clinical manifestations on morphological changes, which not only allows for a correct diagnosis but also for specific therapeutic measures.
Reflex and compression syndromes can be differentiated based on disc herniation, bone growth, and other neural structures that have a pathological effect on the affected spinal structures.
lumbar osteochondrosis syndrome
tocompressionSyndromes that include stretching, squeezing, and deformation of the roots, blood vessels, or spinal cord over designated vertebral structures. toreflectionInclude syndromes caused by the effect of these structures on the receptors that innervate them, primarily the ends of the recurrent spinal nerve (Lushka's disc nerve). The impulse traveling along this nerve from the affected spine reaches the posterior horn of the spinal cord through the posterior root. Switch to the anterior horns, they cause the reflex tension (defense) of the innervated muscles -Reflex tonic disorder.. Switching to its own or adjacent horizontal lateral angle sympathetic center causes reflex vasomotor or dystrophy. This neurodystrophy occurs primarily in hypovascularized tissue (tendons, ligaments) at sites of attachment to bony processes. Here, tissues undergo defibrosis, swelling, and they become painful, especially when stretched and palpated. In some cases, these neurodystrophic disorders cause not only localized pain but also distant pain. In the latter case, the pain is reflected and the affected area appears to "shoot" when touched. Such areas are called trigger areas. Myofascial pain syndrome may occur as part of referred pain of spinal origin.. With chronic tension in the striated muscle, its microcirculation is disturbed in some areas. Sealed areas form in the form of nodules and strands (as well as ligaments) due to hypoxia and edema in the muscle. In this case, the pain is rarely localized, it is not consistent with the innervation area of some roots. Reflex rigidity syndromes, including piriformis syndrome and popliteal fossa syndrome, are described in detail in many manuals.
toLocal (local) pain reflex syndromeIn lumbar osteochondrosis, low back pain is attributed to the acute development of the disease and to low back pain in the subacute or chronic course. An important situation is the established fact thatLow back pain is the result of intradiscal displacement of the nucleus pulposus. Usually, this is a sharp pain that often runs throughout. It can be said that the patient is frozen in an uncomfortable position and unable to straighten. Attempting to change the position of the body can cause an increase in pain. The entire lumbar region becomes immobile, the lordosis flattens, and sometimes scoliosis occurs.
Low back pain - pain, usually pain, aggravated by movement, with axial load. The lower back may be deformed, such as low back pain, but to a lesser extent.
Compression syndromes of lumbar osteochondrosis are also diverse. Among them, nerve root compression syndrome, coccygeal syndrome, and lumbosacral discogenic myelopathy syndrome are distinguished.
nerve root compression syndromeOften develops due to L grade disc herniationFour-LfiveAnd mefive-Sone, because it is at this level that a herniated disc is more likely to develop. Depending on the type of hernia (hole, posterolateral, etc. ), one or the other root will be affected. Typically, one grade corresponds to a single root lesion. Clinical manifestations of root compression LfiveReduced to the appearance of irritation and prolapse in the corresponding dermatomes and hypofunction in the corresponding sarcomeres.
feeling abnormal(numbness, tingling sensation) and shooting pain spread along the outer surface of the thigh, the front surface of the calf to the area of my fingers. Hypoalgesia may then appear in the corresponding area. in the muscles innervated by the root Lfive, especially in the front of the lower leg, with atrophy and weakness. First, weakness is detected in the long extensor muscles of the affected fingers - in muscles innervated only by the root Lfive. The tendon reflexes remained normal in this isolated lesion.
When compressing the spine SoneStimulation and shedding occurred in the corresponding dermatomes, extending to the fifth finger region. Atrophy and weakness primarily cover the posterior muscles of the lower leg. The Achilles tendon reflex is diminished or absent. The knee-jerk reflex is reduced only when the root of the L is involved.2, L3, LFour. Atrophy of the quadriceps, especially the gluteal muscles, also occurs in lumbar disc lesions. Compressed nerve root paresthesias and pain are exacerbated by coughing and sneezing. Movements in the lower back can exacerbate the pain. There are other clinical symptoms that indicate compression of the roots, the development of their tension. The most commonly tested symptoms areLasseger symptomsThe pain in the leg increases dramatically when you try to lift it in a straight state. An unfavorable variant of lumbar vertebral root compression syndrome is cauda equina compression, the so-calledtail syndrome. Most often it develops with a large herniated median disc when all the roots at this level are squeezed. Local diagnosis is made in the upper spine. The pain, which is usually severe, does not spread to one leg, but usually spreads to both, and the loss of sensitivity takes over the area of the rider's pants. Sphincter disorders are added with the rapid development of severe variants and syndromes. Caudal lumbar myelopathy is due to inferior accessory nerve root-medullary artery (usually in the L rootfive, ), manifested as weakness of the fibula, tibia, and gluteal muscles, sometimes with segmental sensory disturbances. Typically, the outer cone segment (L5-Sone) and a cone (S2-S5) spinal cord. In this case, pelvic disease also joins.
In addition to the established primary clinical and neurologic manifestations of lumbar osteochondrosis, there are other symptoms that suggest that this spine has failed. In the context of congenital spinal stenosis and various abnormalities of spinal development, the damage of the intervertebral disc is particularly evident.
Diagnosis of lumbar osteochondrosis
Diagnosis of lumbar osteochondrosisIt is based on the clinical presentation of the disease and other methods of examination, which include routine radiography of the lumbar spine, computed tomography (CT), CT myelography, magnetic resonance imaging (MRI). The diagnosis of lumbar osteochondrosis (PO) has improved significantly as spinal MRI has entered clinical practice. Sagittal and horizontal tomography allows you to see the relationship of the affected disc to surrounding tissue, including assessment of the spinal canal. The size, type, root compression, and structure of a herniated disc. It is important to determine compliance with the level and nature of the major clinical syndromes and lesions. Often, patients with compressed radicular syndrome have a single radiculopathy and the compression of that root is clearly visible on MRI. From a surgical standpoint, this is relevant because. This defines operational access.
Disadvantages of MRI include limitations associated with the examination of claustrophobic patients, as well as the cost of the study itself. CT is a very informative diagnostic method, especially in combination with myelography, but it must be remembered that the scan is performed on a horizontal plane, so the level of the so-called lesion must be determined clinically very accurately. Routine radiography is used as a screening test and is mandatory in a hospital setting. In functional imaging, instability is best defined. Various skeletal dysplasias are also clearly visible on spondylography.
Treatment of lumbar osteochondrosis
For PO, conservative and surgical treatment is performed. existConservative treatmentFor osteochondrosis, the following pathological conditions need to be treated: orthopedic disease, pain syndromes, impaired disc fixation, muscle rigidity disorders, radicular and spinal circulation disorders, nerve conduction disorders, altered scar adhesions, psychosomatic disorders. Conservative treatment (CL) methods include various orthopaedic measures (braking, spinal traction, manual therapy), physiotherapy (therapeutic massage and physiotherapy, acupuncture, electrotherapy), drug prescription. Treatment should be complex and staged. Each CL approach has its own indications and contraindications, but in general, the general approach isAnalgesics, NSAIDs prescription(non-steroidal anti-inflammatory drugs),muscle relaxantandphysiotherapy.
Analgesic effect is achieved by the use of diclofenac, paracetamol, tramadol. Has significant analgesic effecta drugContains 100 mg of diclofenac sodium.
Gradual (long-term) absorption of diclofenac increases the effectiveness of the treatment, prevents possible gastric toxic effects, and makes the treatment as convenient as possible for the patient (only 1-2 tablets per day).
If necessary, increase the daily dose of diclofenac to 150 mg, and prescribe an additional pain reliever in non-long-term tablet form. In milder cases, relatively small doses of the drug are sufficient. In the case of night or morning pain symptoms predominant, it is recommended to take the drug in the evening.
The analgesic activity of the acetaminophen substance is not as good as that of other NSAIDs, so a drug was developed that, along with acetaminophen, includes another non-opioid analgesic, propylphenazone, and mayCodeine and caffeine. In patients with sciatica, reductions in muscle relaxation, anxiety, and depression were seen when caffeine was used. Good results have been achieved in clinical use of the drug for the relief of acute pain in myofascial, rigid and radicular syndromes. Short-term use of the drug is well tolerated and causes few side effects, according to the researchers.
NSAIDs are the most widely used drugs for the treatment of PO. NSAIDs have anti-inflammatory, analgesic, and antipyretic effects and are associated with inhibition of cyclooxygenases (COX-1 and COX-2) - a regulator of the conversion of arachidonic acid to prostaglandins, prostacyclins, thrombosedenzyme. Treatment should always be started with the lowest effective dose of the safest drug (diclofenac, ketoprofen) specified (side effects depend on the dose). For elderly patients and those with risk factors for side effects, initiation of meloxicam therapy, especially celecoxib or diclofenac/misoprostol, is recommended. Other routes of administration (parenteral, rectal) do not prevent gastrointestinal and other side effects. The combination of diclofenac and misoprostol has certain advantages over standard NSAIDs in reducing the risk of COX-dependent side effects. In addition, misoprostol can enhance the analgesic effect of diclofenac.
To eliminate pain associated with increased muscle tone, it is recommended to add central muscle relaxants to the combined treatment:Tizanidine2-4 mg 3-4 times a day or tolperidone 50-100 mg 3 times a day, or tolperidone 100 mg 2 times a day intramuscularly. The mechanism of action of drugs with these substances is significantly different from that of other drugs used to reduce increased muscle tone. Therefore, it is used in cases where other drugs have no antispasmodic effect (in so-called unresponsive situations). The advantage compared to other muscle relaxants for the same indication is that muscle strength is not reduced when muscle tone is reduced in the context of an appointment. The drug is an imidazole derivative, and its effect is related to the stimulation of central a2- Adrenergic receptors. It selectively inhibits the polysynaptic component of the stretch reflex with independent analgesic and mild anti-inflammatory effects. The substance tizanidine acts on spasms of the spinal cord and brain, reducing stretch reflexes and painful muscle spasms. It reduces resistance to passive movement, reduces spasticity and clonic jerks, and increases the strength of voluntary skeletal muscle contractions. It also has gastroprotective properties, which dictate its use in combination with NSAIDs. The drug has few side effects.
OperationFor PO, it progresses with the development of the compression syndrome. It should be noted that the fact that a herniated disc was detected during MRI is not sufficient to make a final decision on surgery. Among patients with radicular symptoms after conservative treatment, up to 85% of patients with a herniated disc do not require surgery. CL, with some exceptions, should be the first step in helping people with PO. If complex CL is ineffective (within 2-3 weeks), patients with disc herniation and radicular symptoms require surgical treatment (CL).
PO has emergency instructions. These include the development of caudal syndrome, often, complete prolapse of the disc into the spinal canal, the development of acute radiculopathy and marked hyperalgesia syndrome, where blockade does not relieve pain even when opioids are prescribed. It should be noted that the absolute size of the disc herniation does not play a decisive role in the final decision on surgery, and should be combined with clinical manifestations, based on the specific conditions observed in the spinal canal on tomography (eg, there may be a smallA combination of hernias and vice versa - hernias are large, but in the middle on the background of a wide spinal canal).
In 95% of disc herniation cases, open spinal access is used. Although many authors have reported their effectiveness, the various discopuncture techniques have not been widely used to date. The procedure is performed using conventional and microsurgical instruments (with optical magnification). During access, bone formation that removes the vertebrae is avoided by primarily using interlaminar access. However, for narrow canal, articular process hypertrophy, and fixed median disc herniation, it is recommended to enlarge the access at the expense of bony structure.
The outcome of surgical treatment depends largely on the surgeon's experience and the correctness of the specific surgical indication. As the renowned neurosurgeon J. Brotchi, who has performed more than a thousand operations on osteochondrosis, aptly put it, "Don't forget that the surgeon must operate on the patient, not on the tomographic images. "
Finally, I would like to re-emphasize the need for a thorough clinical examination and analysis of tomography in order to make the best decision regarding the choice of treatment strategy for a particular patient.














































